3D Printing in Healthcare: Redefining Surgical Outcomes
Personalized medicine is an emerging approach to healthcare that uses an individual's unique physical body and genetic profile to guide decisions made regarding the prevention, diagnosis, and treatment of disease. This approach is based on the understanding that each person's genes, environment, and lifestyle can influence their risk of developing a disease and their response to treatment.

The rise of personalized medicine has been driven by several breakthroughs in technology, including:
- The sequencing of the human genome
- Development of new diagnostic tests
- Development of new therapies
- Advancements in Artificial Intelligence
- The continued maturation of additive manufacturing (AM)
3D Printing in Healthcare and Surgical Planning
Additive manufacturing, also known as 3D printing , is a transformative technology that builds complex 3D objects by layering materials based on digital design files. Digital files pertaining to a patient’s condition can be generated from data obtained through medical diagnostic imaging technologies, such as MRI and CT scans.

Figure 1: A medical technician performing a CT scan on a patient
3D printing is well on its way to helping clinicians, researchers, and medical device manufacturers shape the future of personalized medicine by having a direct positive impact on patient outcomes.
One groundbreaking 3D printing application in healthcare is the rapid production of highly realistic surgical planning models based on a patient’s diagnostic CT scans. These models can be produced to replicate the visual and dimensional characteristics of a specific patient’s tissues, organs, and bones, but also how each of those will feel when the surgeon is cutting or suturing them in the operating room.
Instead of confining themselves to 2D images, 3D printed surgical planning models offer healthcare professionals and their patients a liberating leap into the third dimension. These vivid replicas of a patient's anatomy shed light on hidden complexities, illuminate intricate relationships between organs, and expose the pathology lurking beneath the surface.
This newfound clarity empowers surgeons to make informed decisions with unparalleled confidence, paving the way for better communication with patients and families. But the benefits extend far beyond enhanced understanding.
Surgical planning models become architects of efficiency. By anticipating challenges and charting the optimal path through the intricacies of anatomy, they shave precious minutes off OR time. They serve as invaluable training grounds, allowing a surgical team to rehearse the choreography of the procedure and fine-tune their technique before the real performance. This immersive pre-operative practice fosters seamless teamwork within multidisciplinary teams, ensuring everyone is in perfect harmony on the big day.
However, the stage extends beyond individual surgeries. Planning models open the door to personalized medicine. Physicians can use them in collaboration with biomechanical engineers to craft custom implants or instruments, meticulously designed to fit a patient's unique anatomy. This level of precision can revolutionize surgical outcomes, leading to faster healing and improved quality of life.
Surgical planning models are not just tools; they are gateways to a brighter future of surgery. A future where knowledge illuminates the path, efficiency reigns supreme, and personalized solutions unlock optimal outcomes for each and every patient.

Figure 2: A surgeon uses a 3D printed heart model to test a mitral valve repair prior to treating the patient
Data & Design: Transforming Medical Images Into 3D Reality
One of the bottlenecks in the adoption of 3D printed surgical planning models has been for healthcare institutions sourcing and funding the rapid “segmentation” of data collected from medical imaging scans.
Segmentation is the processing of DICOM data into 3D models. DICOM (Digital Imaging and Communications in Medicine) is the standard format for storing and transmitting medical imaging data. Segmentation involves using sophisticated software to aid clinicians in identifying and delineating specific anatomical structures or regions of interest within the medical images.

Figure 3: With 3D printing, doctors and their patients will no longer have to decipher cryptic images
Segmentation software allows medical imaging specialists to isolate individual components or areas like organs, tumors, or blood vessels in DICOM datasets based on differential tissue density analysis. Once segmented, these regions can then be combined to create detailed 3D representations or models for various purposes, including surgical planning, diagnostics, or research.
When transitioning this data into 3D models for additive manufacturing, accurate segmentation is essential to ensure that the resulting models are a precise reflection of the patient's anatomy. Furthermore, the models will then need to be processed through data manipulation software and build-preparation applications by an experienced technician so that the models present the intended information properly.

Figure 4: A PolyJet 3D printed skull model displaying the extents of a tumor
The Role of Axial3D: Democratizing Personalized Medicine
Axial3D , headquartered in Belfast, Northern Ireland, is a medical technology company that provides cloud-based segmentation and 3D printing services for the healthcare industry with customers in over 30 countries.
The company's founders, Daniel Crawford & Roger Johnston, were motivated to start Axial3D because they saw the potential of additive manufacturing to revolutionize the way that healthcare is delivered. They believed that by making patient-specific 3D models and 3D images more accessible, they could improve the quality of patient care.
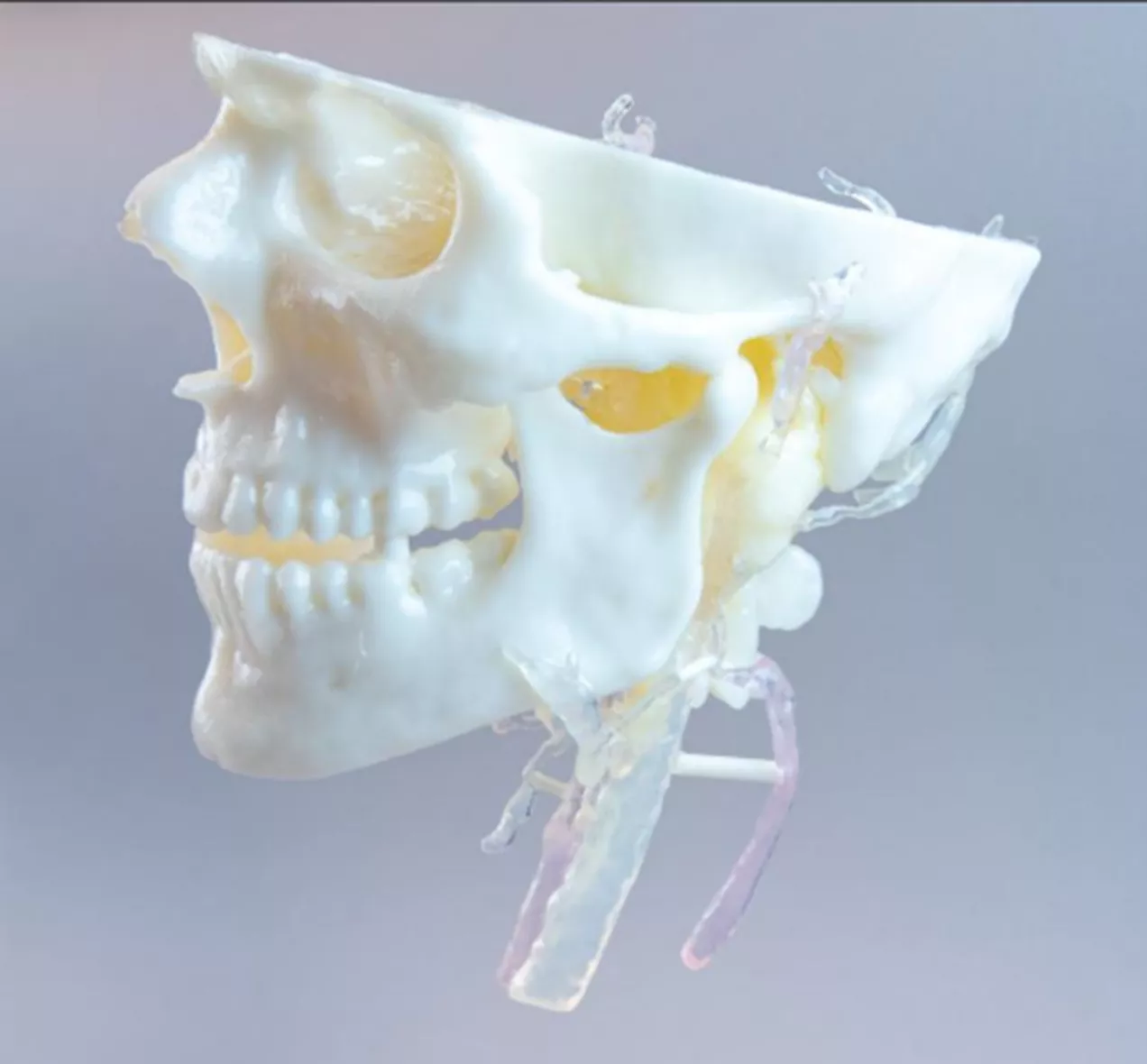
Figure 5: A PolyJet 3D printed Glomus Jugulare Tumor model
Axial3D has since grown to become a leading provider of cloud-based segmentation and 3D printing services for the healthcare industry and has helped to improve the care of thousands of patients.
In 2021, Axial3D was acquired by Stratasys , a leading provider of additive manufacturing solutions. This acquisition has since allowed Axial3D to accelerate its growth and reach even more patients.
Axial3D's Services
Axial3D offers a range of services that can help to improve patient care, including:
- DICOM to 3D conversion : Axial3D can convert medical images from DICOM format to a range of 3D model formats used by 3D printers. This allows medical professionals to create patient-specific 3D models that can be used for planning surgeries, training surgeons, and developing new medical devices.
- Medical image processing : Axial3D can improve the quality of medical images by removing noise and artifacts. This can make it easier to identify features in the images, which can improve the accuracy of the diagnosis and treatment.
- Data analysis : Axial3D can analyze medical data, such as genetic data and lifestyle information. This can help to identify potential risk factors and treatment options.
- Medical device design : Axial3D can assist in the design and manufacture of personalized medical devices and implants. This helps ensure devices are tailored to a patient's needs.
Using Axial 3D: Pixels to Plastic
As an Additive Manufacturing Applications Engineer at GoEngineer, I have tended to gravitate towards medical and dental applications. A couple of years ago, this interest led me to learn how to use segmentation software to process DICOM data into printable 3D models.

Figure 6: (From left to right) A segmented CT scan of an infant’s skull and a printed 3D model generated from the data (segmented, designed and printed by the author)
A colleague recently reached out to me asking for help with a project pertaining to DICOM data. Their surgeon had taken a CT scan of their head during the preparatory phase of their scheduled maxillofacial surgery.
This was an excellent opportunity to try out Axial3D’s service to convert my colleague's DICOM data into a maxillofacial model. The process was easy; I simply uploaded the DICOM files to Axial3D's secure, online platform, and within a few minutes, I had a digital preview of a 3D model of the facial portion of my colleague’s cranium.
The model was accurate and very detailed. I was able to see all of the subtle pits in the bones and the delicate structures and voids in the nasal passages and sinus cavities. The preview looked terrific, so I submitted the file for conversion, and the next day received an email providing me with a link to my finished model!
Figure 7: After uploading the DICOM data to the website, I could see the target geometry within minutes
The model looked great, but I wanted to see if Axial3D could make some changes in how the model was processed. I imagine these types of requests are frequent in a clinical setting. I replied to their email stating it would be helpful if they could add the nose’s cartilage and turbinates (the shell-shaped network of bones, vessels, and tissues within the nasal passages) to the model as a separate solid body so that I could assign different materials to them when the model is being printed on the Stratasys J850 3D printer . The next morning, I had a response from Axial3D and a new file that was exactly what I asked for.

Figure 8: The first printing of my patient-specific maxillofacial model sourced from Axial3D and 3D printed on a
Stratasys J850 Prime
Model Customization and PolyJet Multi-Material 3D Printing
We can now take the model that Axial3D provided and use various software applications to manipulate the data to present it in multiple ways.
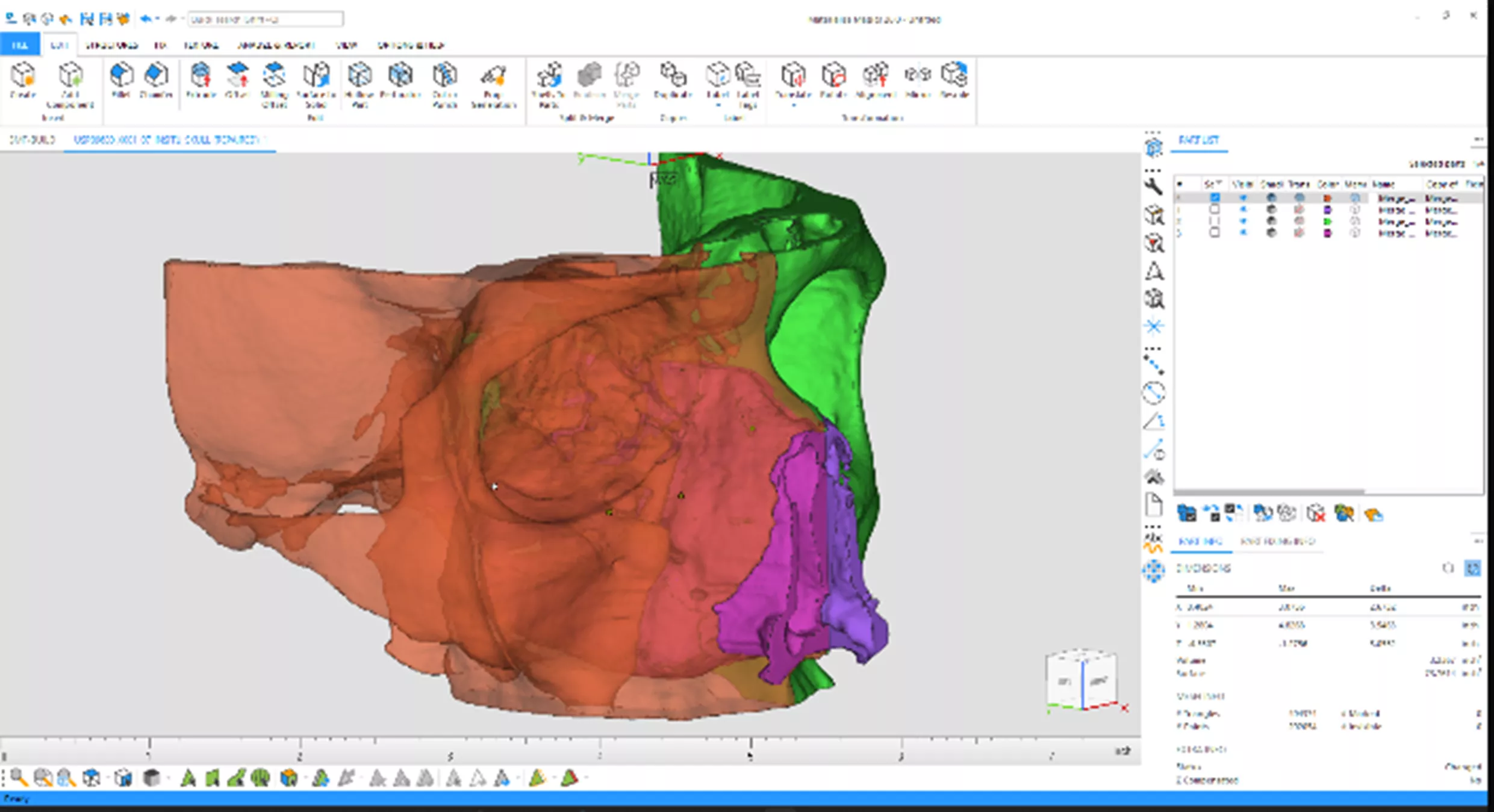
Figure 9: Using
Materialise Magics
, I subdivided the model into different parts and created holes for the installation of magnets to hold the two halves together
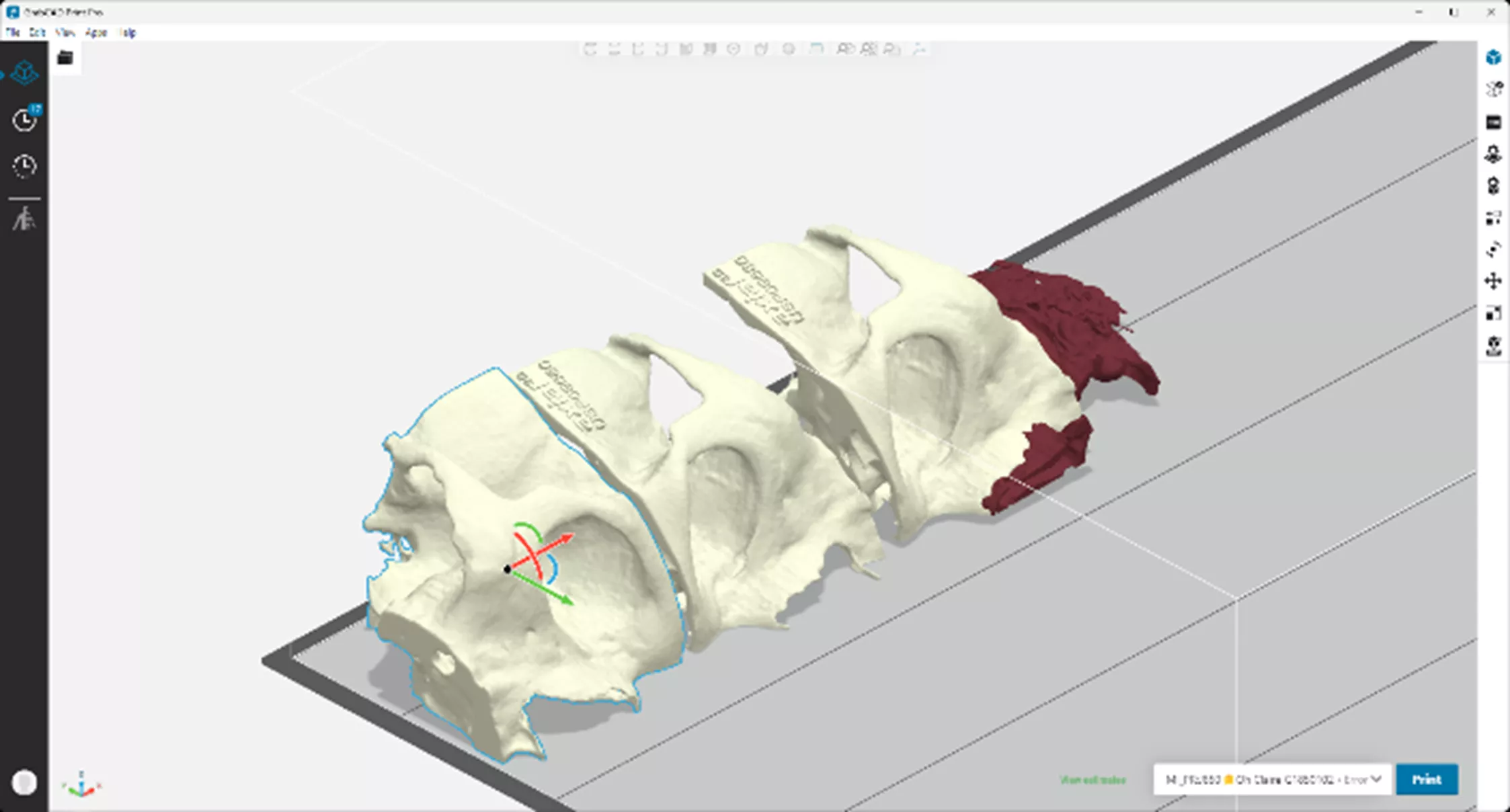
Figure 10: Stratasys's build preparation software,
GrabCAD Print
, allowed me to assign different material properties to the various parts, like color and shore value
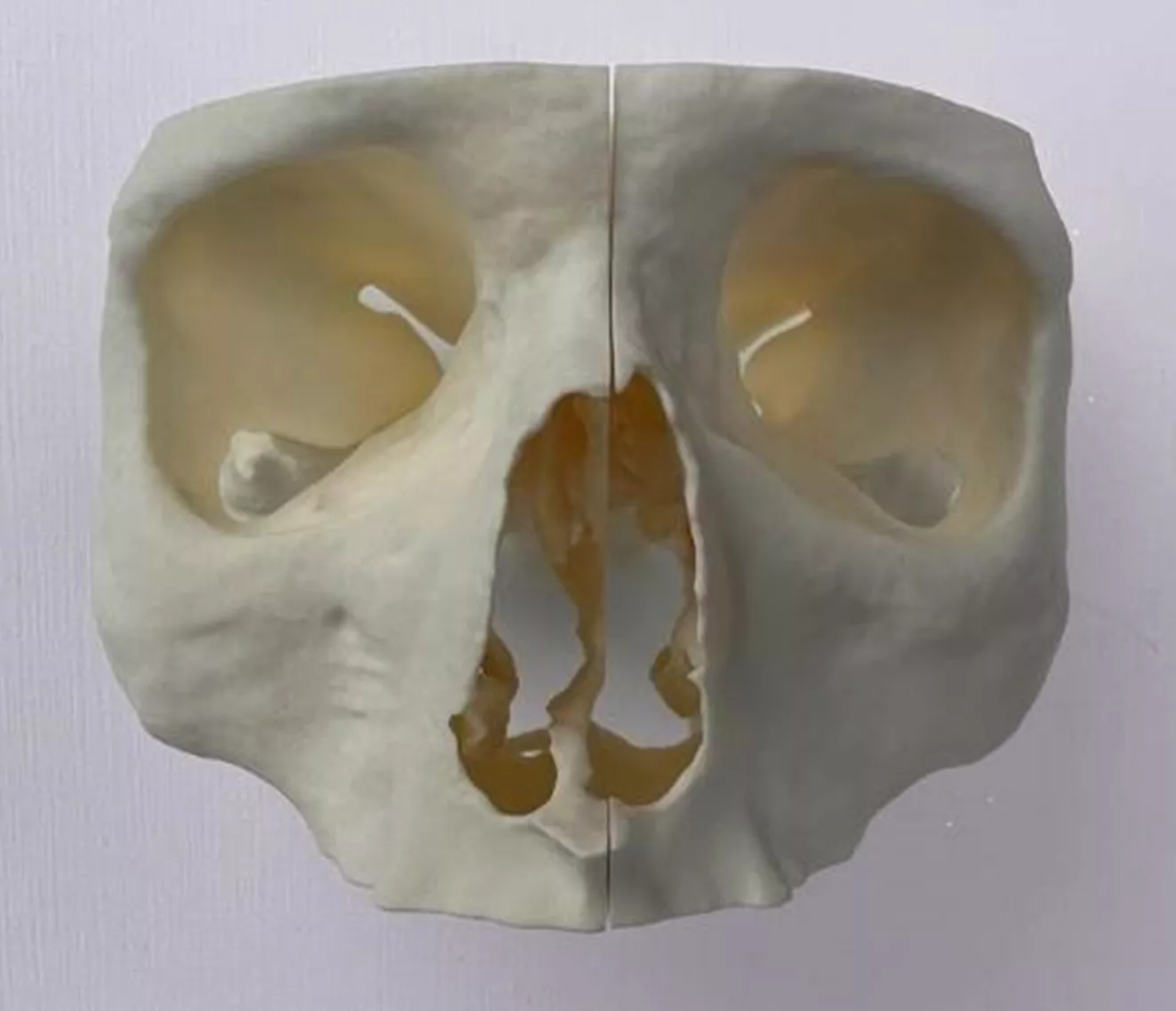
Figure 11: The final printed iteration of my colleague’s maxillofacial model

Figure 12: The model is split in half to expose the interior and is held together with magnets
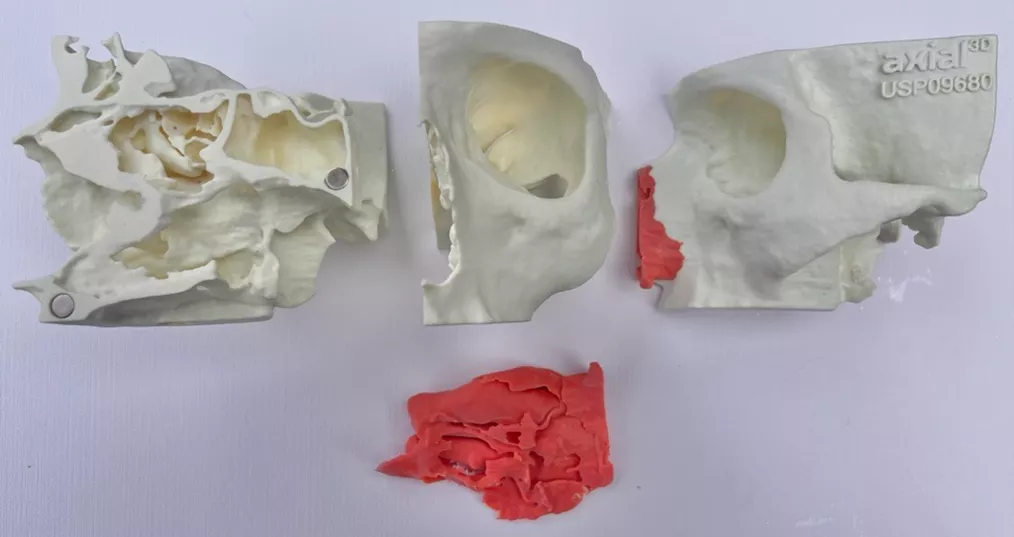
Figure 13: Additional 3D printed variations of the components to allow different model configurations
The Future of Funding: Will 3D Printed Models Become Standard Surgical Equipment?
While 3D printed surgical planning models offer substantial benefits for patient care, insurance reimbursement remains a hurdle. Currently, hospitals utilize temporary Category III CPT codes for billing, which, despite allowing billing, can cause friction with some insurance companies due to their non-permanent status.
In August 2023, the American Academy of Orthopedic Surgeons championed a push for the codes' reclassification to Category I, aiming for wider adoption and smoother reimbursement. The American Medical Association's decision is still awaited, but increased data and advocacy efforts point towards a promising future for this transformative technology in healthcare.
While navigating insurance policies remains crucial, staying informed about upcoming developments will aid hospitals in preparing for potential changes and leveraging 3D printing's full potential to improve patient outcomes.
Unlocking the Future of 3D Printing in Surgery
The future for the continued adoption of 3D printed surgical planning models is bright, but it will take continued effort on the part of clinicians and researchers working together to collect the data required to quantify their positive value to patient outcomes.
Fortunately, companies like GoEngineer, Stratasys, and Axial3D are here to support those efforts. If you are interested in learning more about 3D printing in healthcare and medical applications, contact GoEngineer today.
75% Reduction in Prototyping Costs ⋅ 50% Acceleration in Development time
Download this guide to learn how the medical industry is using 3D printing technology to acceleate time to market, optimize product design, elevate cost efficiencies, and reduce development risk.
More 3D Printing News
Medical 3D Printing: Advanced End-to-End Solutions for Surgeons
Ultimate Guide to PolyJet: Applications, Advantages, History, & More
Experts in Additive: 3D Printing with GoEngineer
Look Inside the New Stratasys J850 Pro Multi-Material PolyJet 3D Printer
GrabCAD Print Pro: Enhance Efficiency & Streamline Workflows

About Richard Cromwell
Richard Cromwell is an Additive Manufacturing Applications Engineer based out of Auburn Hills, MI, having recently joined the team in February 2020. He is a Certified Stratasys Applications Engineer and holds a degree in Technological Science with a specialization in CAD from Oakland Community College in Auburn Hills. Before delving fully into his passion for additive manufacturing and 3D CAD modeling, Richard honed his mechanical design, CAM, and custom fabrication skills while working for over a decade as a renowned craftsman creating custom retrofit piano actions for many of the world’s most prized musical instruments.
Get our wide array of technical resources delivered right to your inbox.
Unsubscribe at any time.